Healthcare providers in United Arab Emirates is going fundamental challenges, altering claim process from traditional paper claims to electronic claims and therefore payers are using data analytics to find any gap to discount the payment.
In this dynamic environment healthcare providers are being challenged to take more on coding and financial risk even they continue to find a way to submit the claims as per regulator requirement
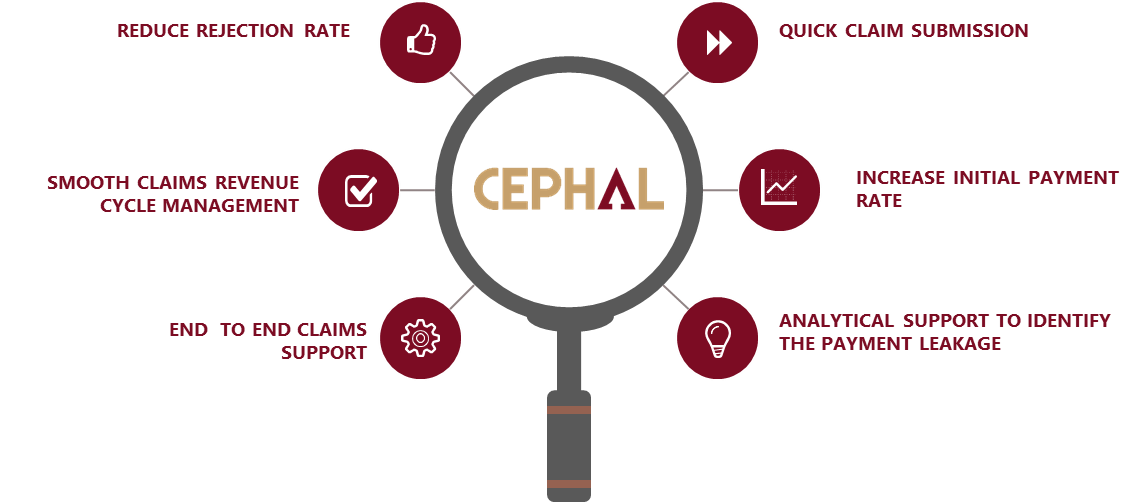
We provide far beyond existing electronic capabilities, enabling organizations to face the above challenges, benefits from high level automation and efficiency that results single submission payment rates for claims, reduce your internal resource cost, increased collection and accelerated cash flow.
Commitment to quality and accuracy is our number one focus. We provide clients with consistent turnaround time on medical coding services. In addition to our in house quality control measures, our HIPAA medical coding services and professional medical coders are also tested regularly with various AHIMA assessments, sample charts, and testing provided by various educational programs..
Simple… We are experts in field of medical billing and practice management. By utilizing our services, your resources can focus on the most important part of your practice – your patients. Our company’s specialty is “medical billing and practice management”. Once you allow us to manage your claims, start to experience the benefits of outsourcing the claims service with a professional team. Our experienced staff has been certified in the field of coding and billing. You will no longer have to worry about the issues such as: staff turnover, tedious claims process and elevated claims rejection rate.
Our fees are set up as a percentage base on claim amount. The cost varies based on the size of the practice and volume of claim..
Assigned to a dedicated Account Executive who will be available to answer any questions or concerns you might have. The burden of the tedious claim process such as Pre-authorization, billing, coding the services and diagnosis, submit the claims within shorter period, and reconcile the payment is now taken away from you and your staff.
Process:We know how important it is for you and your staff to get an update on your patient billing (claim) information! We are proud to offer a seamless connection to Cephal online system at no extra cost!
We offer consultancy service to identity the rejection trend by payer, diagnosis and service and help you to prevent such a rejection.